
Built to support healing.

Elevating the standard for wound care.
Mirragen® is a patented bioactive glass skin substitute made from natural body elements including:
- Boron
- Calcium
- Magnesium
- Phosphorus
It’s engineered for a variety of wound types, from minor to complex. A synthetic material, Mirragen can be stored at room temperature for up to five years, making it an efficient and cost-effective solution for wound care.
A flexible solution for any wound.
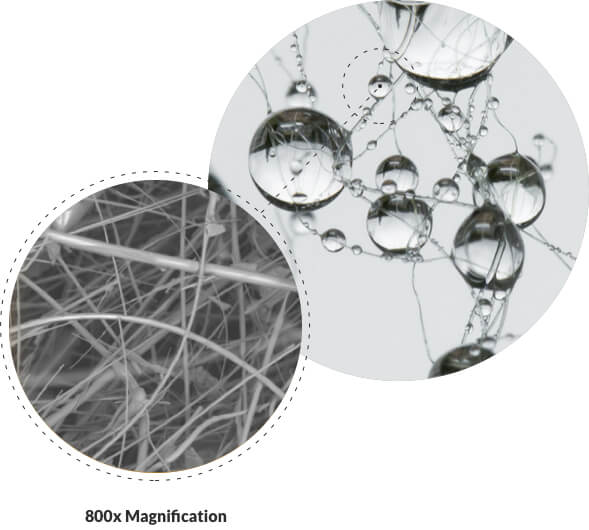
Mirragen has a unique fibrous, flexible structure that makes it easy to form to any wound shape and helps it absorb fluid from the wound bed.
After being placed, Mirragen will slowly dissolve in physiological fluid and is absorbed by tissue surrounding the wound.
Mechanisms of Action
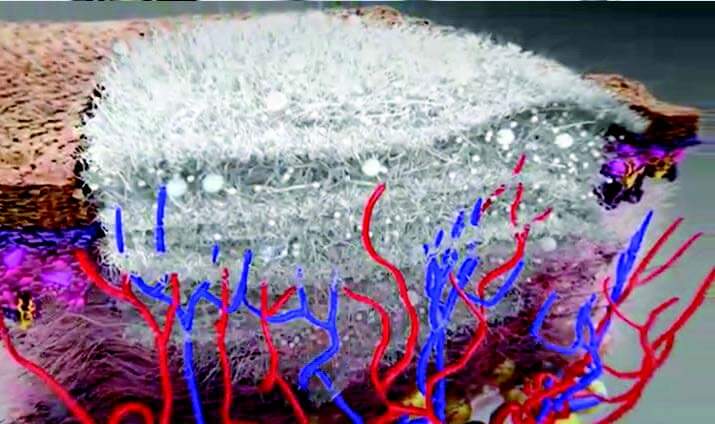
Scaffold Effect of Mirragen

The fiber matrix provides a physical structure – similar to a fibrin clot after hemostasis – for native cells to live, thrive and rebuild tissue.
Those native cells include:
- Endothelial cells that build blood vessels for proper vascularization1
- Fibroblasts that deposit collagen to form granulation tissue2
- Keratinocytes that rebuild the epithelium3
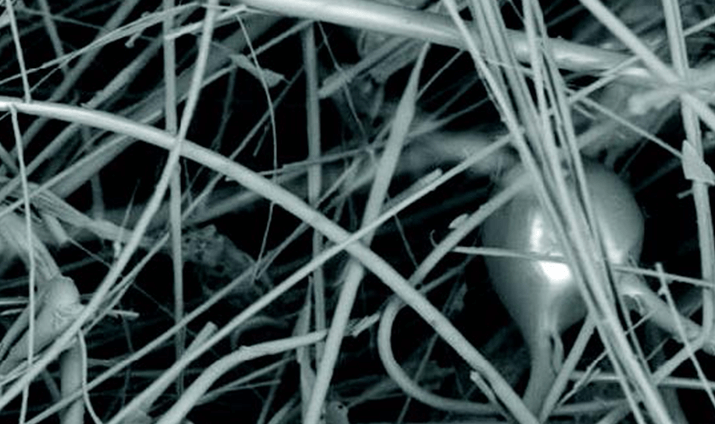
The scaffold’s fibers dissolve over 1-2 weeks, creating space
for native collagen deposition and blood vessel formation
that are essential for granulation tissue.4
The scaffold’s microspheres can persist up to 3 weeks or
longer, continuing to create a sustainable environment
conducive to wound healing.4
Environmental Effect of Mirragen

Mirragen facilitates a wound healing environment conducive to angiogenesis:
- As part of the healing process, the body forms new blood vessels (angiogenesis) through a complex process that includes the secretion of pro-angiogenic factors like VEGF, which facilitates increased migration and proliferation of endothelial cells.5
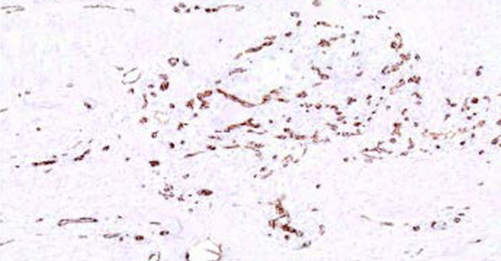
Mirragen
Control
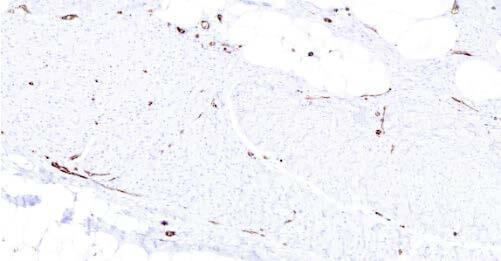
Histology showing blood vessel density at 6 weeks in swine study.
In a swine study, treatment with Mirragen was associated with increased new blood vessel growth compared to control (no treatment).*
1 Krüger-Genge, A., Blocki, A., Franke, R.-P., & Jung, F. (2019). Vascular Endothelial Cell Biology: An Update. International Journal of Molecular Sciences, 20(18), 4411. doi:10.3390/ijms20184411. PMCID: PMC6769656, PMID: 31500313.
2 Tracy, L. E., Minasian, R. A., & Caterson, E. J. (2016). Extracellular Matrix and Dermal Fibroblast Function in the Healing Wound. Advances in Wound Care (New Rochelle), 5(3), 119–136. https://doi.org/10.1089/wound.2014.0561.
3 Piipponen, M., Li, D., & Xu Landén, N. (2020). The Immune Functions of Keratinocytes in Skin Wound Healing. International Journal of Molecular Sciences, 21(22), 8790. https://doi.org/10.3390/ijms21228790. PMCID: PMC7699912. PMID: 33233704.
4 Liu, X., Rahaman, M. N., & Day, D. E. (n.d.). In Vitro Degradation and Conversion of Melt-Derived Microfibrous Borate (13-93B3) Bioactive Glass Doped with Metal Ions. Department of Materials Science and Engineering, and Center for Biomedical Science and Engineering, Missouri University of Science and Technology, Rolla, Missouri 65409.
5 Shi z, Yao C, Shui Y, et al. Research progress on the mechanism of angiogenesis in wound repair and regeneration. Frontiers in Physiology. 2023; 14.
* Data on file.