

Intentionally engineered to
support healing.
Mirragen®, a borate-based bioactive glass fiber matrix facilitates quality tissue formation without the traditional risk of infection tissue-based products have, all in an easy to use, versatile form factor.
The Mirragen Advanced Wound Matrix is intended for use in the management of wounds. Wound types include: Partial and full-thickness wounds, pressure ulcers, venous ulcers, diabetic ulcers, chronic vascular ulcers, tunneled/ undermined wounds, surgical wounds (donor sites/grafts, post-Moh’s surgery, post laser surgery, podiatric, wound dehiscence), trauma wounds (abrasions, lacerations, first and second degree burns, skin tears) and draining wounds.

- Granulation: supports blood vessels and collagen for strong, resilient tissue.

Without the traditional risk of infection tissue-based products have.
- In an RCT, the Mirragen group experienced no adverse events related to infection of the index ulcer.
- The SOC group, a collagen alginate, had a 25% infection rate.1

All in an easy to use, versatile form factor.
- Adaptable to all wound shapes – no need for preparation or thawing.
- Stays in place even in deeper or tunneling wounds.
- Stored at room temperature for up to five years.

Empowering the body to heal itself.
Mirragen® is an intentionally engineered porous scaffold made of bioactive glass fibers and microspheres, designed to create an ideal environment that supports the wound healing process. Unlike typical glass, bioactive glass is a soft, fibrous material that conforms to the wound. It is composed of elements naturally found in your body. As your wound improves, Mirragen is absorbed into the surrounding tissue, eliminating the need for removal.
Designed for clinical efficiency.
Mirragen is supplied in a protective tray inside a sealed sterile pouch. It requires no preparation steps prior to use. Simply open the package and apply to the wound. Mirragen can be stored at room temperature for up to five years, helping to simplify logistics in the clinical setting.
| Size (Metric) | Product No. | Units/Box |
|---|---|---|
| 1.5 × 1.5 cm | MWM-015-015BX | 10 |
| 2.5 × 2.5 cm | MWM-025-025BX | 10 |
| 3.5 × 3.5 cm | MWM-035-035BX | 10 |
| 4.5 × 4.5 cm | MWM-045-045BX | 10 |
| Size (Metric) | Product No. | Units/Box |
|---|---|---|
| 1.5 × 1.5 cm | MWM-015-015EA | 1 |
| 2.5 × 2.5 cm | MWM-025-025EA | 1 |
| 3.5 × 3.5 cm | MWM-035-035EA | 1 |
| 4.5 × 4.5 cm | MWM-045-045EA | 1 |
*5.1 x 5.1 cm size discontinued in 2024

Empower the body to heal itself


Surgical Dehiscence – Trans Metatarsal Amputation
(64-year-old male)
The wound fully closed after only six applications of Mirragen® Advanced Wound Matrix within 42 days. Individual results may vary.
History of diabetes and neuropathy. Prior treatments included three surgical closure attempts, two failed skin substitute products and one amnion graft. Individual results may vary.
Mirragen is effective and safe for a range of wounds.
Venous ulcers
Pressure ulcers
Surgical wounds
(Donor sites/grafts, post- Mohs surgery, post-debridement, dehiscence)
Trauma wounds
(Abrasions, lacerations, first- and second-degree burns, skin tears)
Partial and full-thickness wounds
Diabetic ulcers
Podiatric, wound dehiscence
Atypical wounds
(Pyoderma gangrenosum, tunneling, undermining)
Lower risk of infection relative to tissue-based products
Pathogen Interaction with Collagen-Based Products:
Many gram-positive pathogens found in diabetic foot ulcers, such as Staphylococcus aureus, Enterococcus faecalis, and Streptococcus equi, can bind to collagen using collagen-binding adhesins.2,3,4
Sources and Vulnerability of Collagen:
Collagen can be extracted from various sources such as porcine, bovine, avian, and piscine tissues. Despite its useful properties, crude natural collagen can be easily colonized and degraded by bacteria and fungi.10
I have used Mirragen on one of my most difficult cases where other skin substitutes did not work. I am impressed by Mirragen, and I have not been impressed in a long time.
Dr. Laurentin Perez
Multicenter Randomized Controlled Trial
Study comparing Mirragen plus SOC to SOC alone for the treatment of diabetic foot ulcers. After two weeks of screening, patients are randomized for 12 week treatment. For this patient population, Mirragen had the greatest impact during first 4 weeks of treatment.1
79.4% vs. 36.5%

Mirragen doubled the SOC (Standard of Care) in wound area reduction (79.4% vs 36.5%)
2.8x

Mirragen increased wound closure 2.8x vs. SOC
0 infections

SOC had 5 patients withdrawn due to infection, Mirragen had 0 adverse events related to infection of the index ulcer.
Mechanisms of Action
Scaffold Effect of Mirragen

The fiber matrix provides a physical structure – similar to a fibrin clot after hemostasis – for native cells to live, thrive and rebuild tissue.
Those native cells include:
- Endothelial cells that build blood vessels for proper vascularization5
- Fibroblasts that deposit collagen to form granulation tissue6
- Keratinocytes that rebuild the epithelium7
The scaffold’s fibers dissolve over 1-2 weeks, creating space
for native collagen deposition and blood vessel formation
that are essential for granulation tissue.8
The scaffold’s microspheres can persist up to 3 weeks or
longer, continuing to create a sustainable environment
conducive to wound healing.8
Environmental Effect of Mirragen

Mirragen facilitates a wound healing environment conducive to angiogenesis:
- As part of the healing process, the body forms new blood vessels (angiogenesis) through a complex process that includes the secretion of pro-angiogenic factors like VEGF, which facilitates increased migration and proliferation of endothelial cells.9
Mirragen
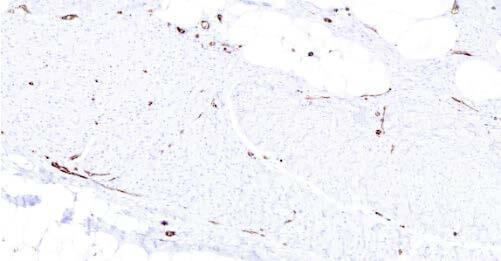
Control
Histology showing blood vessel density at 6 weeks in swine study.
In a swine study, treatment with Mirragen was associated with increased new blood vessel growth compared to control (no treatment).*
Resources and Downloads
1 Armstrong DG, Orgill DP, Galiano RD, et al. A multi-centre, single-blinded randomized controlled clinical trial evaluating the effect of resorbable glass fibre matrix in the treatment of diabetic foot ulcers. Int Wound J. 2021;1-11.
2 Lannergafird, J., Frykberg, L., & Guss, B. (2003). CNE, a collagen-binding protein of Streptococcus equi. Department of Microbiology, Swedish University of Agricultural Sciences, P.O. Box 7025, 750 07 Uppsala, Sweden. Accepted 19 March 2003, First published online 8 April 2003.
3 Patti JM, Boles JO, Hook M. Identification and Biochemical Characterization of the Ligand Binding Domain of the Collagen Adhesin from Staphylococcus aureus. Institute of Biosciences and Technology, Center for Extracellular Matrix Biology, Texas A&M University, Houston, Texas 77030. Received June 1, 1993; Revised Manuscript Received August 10, 1993.
4 Rich, R. L., Kreikemeyer, B., Owens, R. T., LaBrenz, S., Narayana, S. V. L., Weinstock, G. M., Murray, B. E., & Ho¨o¨k, M. (1999). Ace Is a Collagen-binding MSCRAMM from Enterococcus faecalis. Received for publication, March 30, 1999, and in revised form, May 6, 1999.
5 Krüger-Genge, A., Blocki, A., Franke, R.-P., & Jung, F. (2019). Vascular Endothelial Cell Biology: An Update. International Journal of Molecular Sciences, 20(18), 4411. doi:10.3390/ijms20184411. PMCID: PMC6769656, PMID: 31500313.
6 Tracy, L. E., Minasian, R. A., & Caterson, E. J. (2016). Extracellular Matrix and Dermal Fibroblast Function in the Healing Wound. Advances in Wound Care (New Rochelle), 5(3), 119–136. https://doi.org/10.1089/wound.2014.0561.
7 Piipponen, M., Li, D., & Xu Landén, N. (2020). The Immune Functions of Keratinocytes in Skin Wound Healing. International Journal of Molecular Sciences, 21(22), 8790. https://doi.org/10.3390/ijms21228790. PMCID: PMC7699912. PMID: 33233704.
8 Liu, X., Rahaman, M. N., & Day, D. E. (n.d.). In Vitro Degradation and Conversion of Melt-Derived Microfibrous Borate (13-93B3) Bioactive Glass Doped with Metal Ions. Department of Materials Science and Engineering, and Center for Biomedical Science and Engineering, Missouri University of Science and Technology, Rolla, Missouri 65409.
9 Shi z, Yao C, Shui Y, et al. Research progress on the mechanism of angiogenesis in wound repair and regeneration. Frontiers in Physiology. 2023; 14.
10 Warowicka, A., Kościński, M., Waszczyk, M. et al. Berberine and its derivatives in collagen matrices as antimicrobial agents. MRS Communications 12, 336–342 (2022). https://doi.org/10.1557/s43579-022-00181-w
* Data on file.