Treating A Challenging Hysterectomy Wound
Even though Laurie H. says “I don’t heal well” when talking about her medical past, it was a different story when she turned to Mirragen® to help close a difficult wound.
The story for this Registered Nurse in the Surgical Intensive Care Unit at Vanderbilt, often referred to as the “wound guru” and “ostomy queen”, begins when she had what was supposed to be a simple vaginal hysterectomy in 2010.
Three weeks after her operation, Laurie became acutely septic when an abscessed ovary ruptured, requiring multiple hospitalizations and eventually an additional surgery for wash out. In 2019, she had a small bowel obstruction where a tiny diverticulum got stuck in some of those adhesions from the surgeries in 2010. After a bowel resection, her wound closure took months.
Despite closure, her wound continued to cause issues and in 2019 where the wound had dehisced, Laurie developed a peri-umbilical hernia and a massive ventral hernia.
“Between 2019 and 2022, I had multiple ER visits and hospital admissions (at least 3-5 per year) for more small bowel obstructions, where a loop of bowel would get stuck in one of those hernias, usually the smaller peri-umbilical one,” said Laurie.
Laurie somehow managed to avoid surgery, but in December of 2022 she was not so fortunate. She developed yet another bowel obstruction that wouldn’t cooperate and decompress, so Laurie had surgery to repair a total of three hernias with a macropore mesh.
Post op she had a little bit of leaking between staples, but by three weeks the staples were out, the drain was removed, and the incision stopped leaking.
“I was so thrilled to go to bed without needing a dressing,” said Laurie.
However, by the third week Laurie quickly began seeing drainage from the wound and she ended up back in the ER.
“In the coming days, I had an I&D surgery and was discharged home with a wound vac and home health care,” said Laurie. “I ran out of sick time, vacation time, and even FMLA, so I went back to work in the Vanderbilt SICU with my wound vac on me like a fanny pack, tucking the tubing underneath my scrubs.”
By mid-March, the wound opening got so tiny that doctors couldn’t get a sponge in it for the wound vac, but it still tunneled several centimeters.
“By mid-April, it was clear we weren’t making progress,” said Laurie. “Drainage was turning green, I think it tunneled about 4cm, so another I&D surgery was done and a tiny portion of the mesh was removed.”
After a month, the wound opening got tiny again, so tiny that they couldn’t use the wound vac any longer and had to go back to packing it with gauze strips. Over the coming months, Laurie’s wound would need to be packed with ¼” gauze strips every 12 hours.
By November 2023, conversations started again about needing to repeat an I&D surgery. Laurie wanted a second opinion from the Wound team and saw the MD who was the head of that department. His recommendation was also another I&D, plus admission to the hospital for several days of Vera Flow wound vac, then go home with a wound vac.
“I did NOT want another surgery, and we were approaching the holidays yet again, but at this point my wound, only a few millimeters at the opening, was tracking about 7cm,” said Laurie. “I remember pulling out that long piece of packing strip gauze, holding it at my waist and it reached the floor. I reached a point where I was trying to decide just how okay I was with the potential reality of packing my abdomen twice a day for the rest of my life, because even with another surgery I was sure that this was the trajectory of events.”
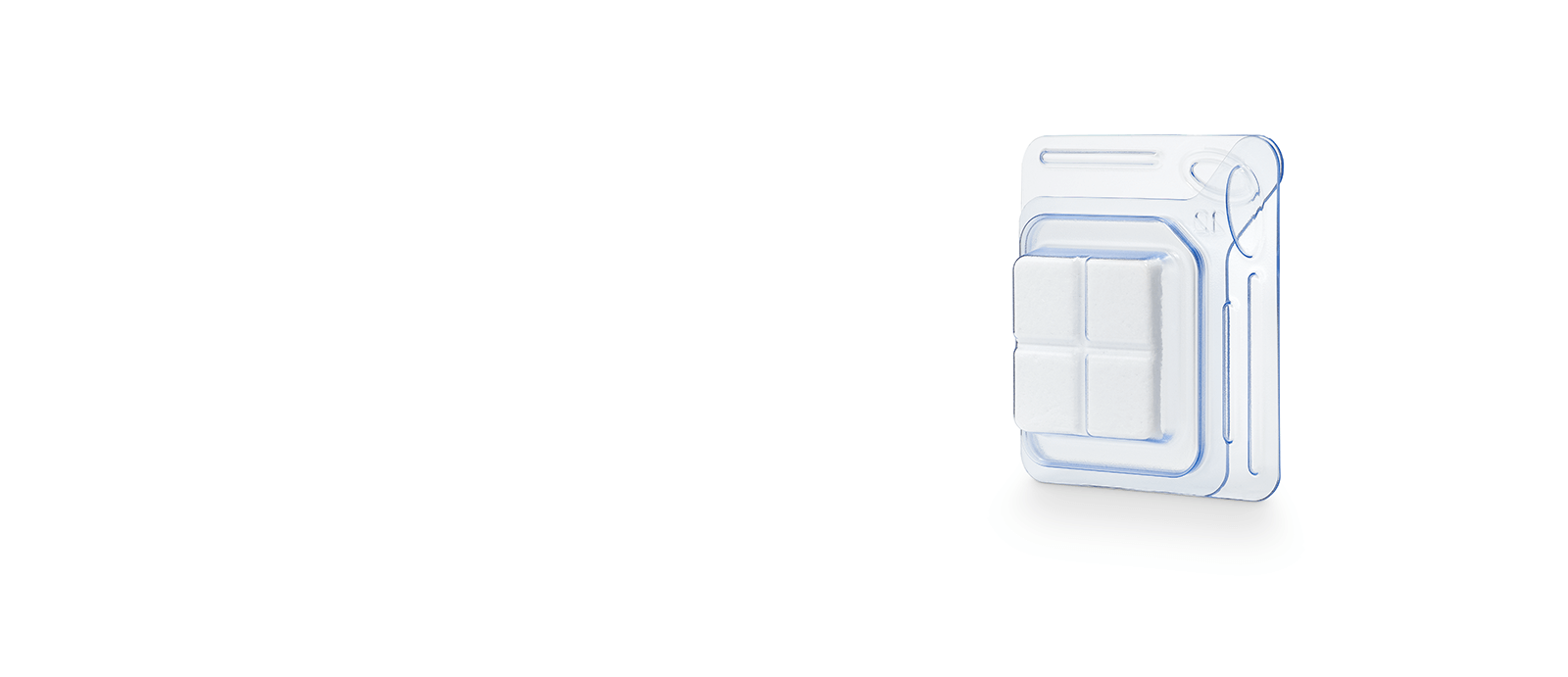
Just when things were bleak for Laurie, a former co-worker introduced her to Mirragen, which he thought could significantly help. For Laurie, hearing bioactive glass made her think he wanted to put fiberglass in her wound.
“At this point, facing another cycle of surgery, wound vac, and dressings, I was willing to try ANYTHING…hyperbaric oxygen therapy, weird honey, magic beans, ANYTHING,” said Laurie.
Fast forward to mid-December, Laurie received her first application of Mirragen when her wound measured 7.5 cm deep.
“I enjoyed a blissful week of NO dressing changes, no wound vac, and when I returned the following week the wound depth had decreased by more than half,” Laurie said.
I enjoyed a blissful week of NO dressing changes, no wound vac, and when I returned the following week the wound depth had decreased by more than half.”
Laurie H. (after receiving Mirragen for the first time)
While progression turned a little slower, doctors have adapted the dressing changes to add a few drops of saline since the wound isn’t producing much exudate, and they started packing Mirragen more loosely to allow more space for granulation. As of now, the wound opening is SO tiny you can barely see it, tunneling around 1 cm.
“Progress is slow, but it is still progress that I have not experienced with any other treatment to date,” Laurie said. “I go to the clinic weekly for additional Mirragen application, but that is only one dressing change per week, whereas I had previously been doing 28 per week. There hasn’t been any pain before or during Mirragen use, so that hasn’t changed. My wound hardly tunnels and is the smallest it has ever been, has zero odor, no green exudate.”
Various providers have since commented on how fast and simple the reapplication process of Mirragen is since there is nothing to remove, debride, or even irrigate. More importantly, Laurie has seen no negative side effects from using Mirragen.
“As an RN that sees ‘the worst of the worst’ wounds, I can only wonder how some of my patients could have benefited from using this product, especially those patients with devastating necrotizing fasciitis wounds that require at least daily dressing changes, if not more frequently,” said Laurie. “I hope that my facility will quickly approve the use of this product, as I am anxious to teach my coworkers about it, but even more excited for the hope it can bring to my patients.”
As an RN that sees ‘the worst of the worst’ wounds, I can only wonder how some of my patients could have benefited from using this product, especially those patients with devastating necrotizing fasciitis wounds that require at least daily dressing changes, if not more frequently.
Laurie H.